Medical Treatments
- Urology Treatment
- Bariatric Obesity Surgery
- Oncology Cancer Treatment
- Cardiology
- Cosmetic Plastic Surgery
- ENT-Head And Neck Surgery
- Infertility Or IVF Treatment
- Joint Replacement Surgery
- Spine Surgery
- Organ Transplant
- Neurology
- Orthopedic Surgery
- Nephrology
- Stem Cell Therapy
- Endocrionology Or Diabetes
- 3D Liposuction Abdomen Lower Back
- Breast Lifting Implant
- Paediatrics Child Neonate
- Robotic Surgery
- Dentistry Dental Implant
- Gynaecology
- Pulmonology /Chest /Respiratory
- Dermatology And Venerelogy
- Opthalmology Eye Treatment
- Gastroenterology Or Hepatology
- Cyber Knife Radiosurgery
- Bone Marrow Surgery Transplant
Bone Marrow Surgery Transplant
Bone Marrow Transplant for Sickle Cell Anemia Treatment
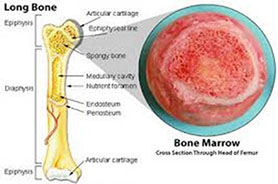
Bone marrow transplant of stem cell transplantation is a potential cure for sickle cell disease. Stem cells are cells which are normally found in bone marrow. Bone marrow is basically a substance which is located in the center of bones & which is found to produce red blood cells found in blood. Patients with sickle cell disease have bone marrow which produces red blood cells having defective hemoglobin S. But when, this bone marrow is replaced with healthy bone marrow, the patient is found to start producing normal hemoglobin. When stem cell transplants require from another person known as a donor, it is known as allogeneic stem cell transplantation. Bone marrow cells are taken from someone else before the transplant having closely matching bone marrow. This is most often a healthy sister or a brother. The child suffering from sickle cell disease is now treated with drugs which destroy their bone marrow cells after which the donated bone marrow stem cells are injected into the patients’ vein. After completion of this process, the donated bone marrow starts to replace the bone marrow of the recipient. The new cells are meant to restore the immune system of the patient & thereby produce normal red blood cells.
What is Sickle Cell Disease?
Red blood cells are produced with the bone marrow. The unique biconcave shape of red blood cells increases the storage capacity of the hemoglobin molecules which eventually would carry oxygen. Red blood cells are also soft & pliable so that they can squeeze through the tiniest blood vessels within the body. However, in sickle cell disease patients, these red blood cells form abnormal crescent shape & which is rigid. This causes the red blood cells to be damaged. Sickle cells are not malleable so as to squeeze through tight spaces. This can eventually increase risk of formation of blood clots within small size capillaries of different organs & which can cause potential for damage to organs.
Some Facts Regarding Sickle Cell Anemia
• Sickle cell anemia or sickle cell disease (SCD) is a disorder which is inherited & relates to the hemoglobin in blood.
• Inheritance of two sickle cell genes is required for sickle cell anemia.
• Inheritance of one sickle cell gene is known as sickle cell trait almost never causes any problems.
• Virtually all major symptoms of sickle cell disease are the direct result of abnormally shaped & sickled red blood cells blocking blood flow in bloodstream.
• Current treatment option of sickle cell anemia is primarily directed towards managing individual features of disease as they occur.
More about Sickle Cell Disease
Sickle cell disease or sickle cell anemia is a disorder of blood which is caused by inherited abnormal hemoglobin which is the oxygen-carrying protein within the red blood cell. This abnormal hemoglobin subsequently causes distorted or sickled red blood cells within the patient. Sickled red blood cells are fragile & often prone to rupture as well. Sickle cell anemia results when number of red blood cells is found to decrease from hemolysis or rupture. This is the condition which is medically referred to as sickle cell disease or sickle cell anemia. Subsequently, it is possible that irregular sickled cells block blood vessels so as to cause tissue & organ damage along with pain. Sickle cell disease is one of the most common blood anemia’s which is inherited. This disease is primarily found to affect Africans & African Americans in general. It is estimated that more than 90,000 to 100,000 Americans are afflicted with sickle cell disease. Current estimates indicate that at least one in every 500 African American citizens in the United States is affected with sickle cell disease.
Inheriting Sickle Cell Disease
Inherited as an autosomal recessive condition, sickle cell disease gene is not linked to the sex chromosome. It means that this gene can be passed on from a parent & can carry to both the female & the male child. However, a sickle gene must be inherited from both the father & the mother for sickle cell anemia to occur. This means that the child must have two sickle cell genes for sickle cell disease to happen. Inheritance of a single sickle gene is medically termed as sickle cell trait or a ‘carrier’ state. Nevertheless, sickle cell trait will not cause sickle cell disease. People with sickle cell trait will usually not have many symptoms of sickle cell disease & will also have identical life expectancies & hospitalization rates quite similar to unaffected people. However, whenever two carriers of sickle cell trait would mate, it is like to have a one in four chance that the offspring will have sickle cell anemia. In quite a few parts in Africa, one in every five individuals is found to be a carrier of sickle cell trait.
Conditions Promoting Sickling of red Blood Cells in SCD Patients
Sickling of red blood cells among patients with sickle cell disease eventually result in cells with abnormal shape along with diminished flexibility. Moreover, sickling is also promoted by conditions which are associated with low levels of oxygen, increase in acidity & dehydration of blood. These conditions normally occur from injuries to body tissues, or dehydration or use of anesthesia. Moreover, certain organs of the patients body are predisposed to acidity or lower levels of oxygen like when blood moving in kidney, spleen, or liver at a slower pace. Other organs, particularly with high metabolism rates, like muscles, brain & placenta in pregnant women with sickle cell disease, promote further sickling by extracting additional oxygen from blood. These conditions generally make the patient’s organs more susceptible to injury from sickle cell disease.
Diagnosing Sickle Cell Anemia
Sickle cell disease is suggested when abnormal sickle-shaped cells in blood are identified under microscope. Typically, testing is performed on a smear of blood using special low-oxygen preparation referred to as sickle prep. Other prep tests which are utilized to detect abnormal hemoglobin S include solubility tests performed on tubes of blood solutions. Sickle cell disease can be confirmed by specifically quantifying types of hemoglobin which are present by using hemoglobin electrophoresis tests. Prenatal diagnosis or before birth diagnosis of sickle cell anemia is also possible by using chorionic villus sampling or amniocentesis tests. The sample which is obtained is subsequently tested for DNA analysis of fetal cells. Hemoglobin electrophoresis test precisely identifies hemoglobins in blood by separating them. This separation of different hemoglobins is possible due to the unique electrical charge each one of them have upon their protein surfaces & which cause them to move characteristically in electric fields while they are tested in a laboratory.
Signs & Symptoms of Sickle Cell Disease
All major signs & symptoms of sickle cell disease are direct result of abnormally shaped & sickled red blood cells which block flow of blood circulating through tissues of the body. These tissues with impaired circulation suffer damage due to lack of oxygen. Damage to organs & these tissues of the body can cause severe disability among patients with sickle cell disease. These patients end up enduring episodes of intermittent crises of variable severity & frequency which depends upon the degree of organ involvement. Major features & signs & symptoms of sickle cell disease include the following.
• Pain Crises
• Anemia & Fatigue
• Bacterial Infections
• Arthritis & Dactylitis (inflammation & swelling of hands and/or feet)
• Injury to Heart & Lungs
• Liver Congestion & Splenic Sequestration (sudden pooling of blood in spleen)
• Ulcers in Leg
• Aseptic Necrosis & Bone Infarcts (death of parts of bone)
• Damage to Eyes
• Other Features
Some features of sickle cell disease like anemia, fatigue, bone infarcts & pain crises can occur at any age. Several features typically occur in certain age groups of patients.
Sickle cell disease generally first presents itself in the first year of life. Infants & young children usually suffer with fever, splenic sequestration, dactylitis or painful swell of hands & feet, pneumococcal bacterial infections & abdominal pain. Adolescents & young adults are more commonly found to develop aseptic necrosis, leg ulcers & damage to the eye. Signs & symptoms in adults are typically intermittent episodes of pain due to injury of muscle, bone or internal organs. Affected infants however do not develop signs & symptoms within the first few months of life due to the fact that fetal hemoglobin or hemoglobin produced by developing fetus protects red blood cells from getting sickled. Fetal hemoglobin is however absent in red blood cells which are produced after birth & therefore by 5 months of age sickling of red blood cells is prominent & signs & symptoms begin to appear.
Treatment of sickle cell disease is usually directed towards individual features of illness which are present in the patient. Generally, treatment is directed at management & prevention of acute manifestations & therapies which are directed towards blocking red blood cells from stacking together. However, there is no single remedy to reverse the disease. Therefore, it is very important that the affected individual including the family members have optimal understanding of illness & they effectively maintain communication with doctors & the healthcare team.
• Anemia & Fatigue
Fatigue is a very common symptom among people with sickle cell disease. Sickle cell disease is found to cause a chronic form of anemia which would eventually lead to fatigue. Red blood cells of sickle cell disease patients are prone to hemolysis (breakage) & which in turn causes a reduced life span of red blood cells, whereas a normal life span of red blood cells is around 120 days. However, these sickled red blood cells are very easily detected under microscopic examination of smear of blood on glass slides. Site of production of red blood cells is bone marrow & which typically works overtime to rapidly produce more cells so as to compensate destruction of sickled red blood cells in the blood circulation. However, bone marrow also sometimes suddenly stops producing red blood cells & which can cause a very severe type of anemia known as aplastic crises. These aplastic crises are usually promoted by infections which otherwise in normal circumstances would seem to be less significant, including viruses of stomach & bowels & influenza. Anemia of sickle cell disease also tends to stabilize without any specific treatments. Degree of sickle cell disease anemia is defined by measurement of hemoglobin levels in blood. Hemoglobin basically is the protein molecule within red blood cells that carry oxygen from lungs to tissues of the body & also return carbon dioxide from tissues to lungs. Blood hemoglobin levels among persons with sickle cell disease are generally in-between 6 – 8 gms/dl whereas normal levels are above 1 gms/dl. Occasionally, there also are severe drops in hemoglobin among sickle cell disease patients which require blood transfusions so as to correct anemia. This is particularly so in SCD patients suffering splenic sequestration. Blood transfusion among SCD patients is usually reserved for those with other complications like late pregnancy, severe leg ulceration, stroke, lung infarction & pneumonia. Risks of blood transfusion among SCD patients include injury to body tissues due to iron overload, immune reaction, infection & hepatitis. Blood transfusions are also provided to SCD patients preparing for surgical interventions. Folic acid is also given to SCD patients as a supplement & in some cases red blood cell exchange is also performed. However, this procedure is also able to remove some sickle blood cells & replace them with non-sickle normal blood cells. This is usually performed when sickle cell crisis is so severe that any other form of treatment is unable to help.
• Pain Crises
Pain crises in people with sickle cell disease are intermittent painful episodes resulting from inadequate blood supply to body tissues. Impaired circulation is generally caused by blockage of many blood vessels from sickling of red blood cells. Sickled red blood cells either slow down or completely impede normal flow of blood through tissues. Eventually, this leads to excruciating pain which often requires hospitalization & opiate medications for providing relief. Typically, this pain is throbbing pain & can shift location from one area of the body to another. Moreover, bones are also frequently affected. Pain in abdomen is also common & can often mimic appendicitis. Quite often, fever is associated with episodes of pain crises. Pain crisis is also promoted by preceding dehydration, injury, infection, exposure to cold, emotional stress or strenuous exercising. People with sickle cell disease should therefore avoid extremes of cold & hot as a preventive measure. These pain crises episodes usually require analgesia for pain relief along with increased intake of fluids. Dehydration should be prevented so as to avoid further injury to tissues while intravenous fluids can often be necessary. Clotrimazole along with fluids & magnesium are also most often given. Other modalities which can be helpful in these episodes include self-hypnosis, electrical nerve stimulation & biofeedback. Hydroxyurea is also another medication which is currently being used in children & adults with severe pain resulting from sickle cell disease pain crises. This medication is also considered for those patients who have had frequent transfusions & recurrent strokes. This drug is designed to act by increasing amount of fetal hemoglobin in blood which is quite resistant to sickling of red blood cells. However, patient response to hydroxyurea is unpredictable & variable from one patient to another. Moreover, hydroxyurea can also be suppressive to bone marrow.
• Arthritis & Dactylitis
Inflammation & swelling of feet and/or hands is often an early sign & symptom of sickle cell disease. This swelling usually involves the entire fingers including toes sometimes. This condition is medically termed dactylitis. Dactylitis is most often caused by injury to bones of affected digits which are caused by repeated episodes of inadequacy of circulation in blood. Dactylitis is generally found to occur among children with sickle cell disease aged in between 6 months to 8 years of age. Arthritis or joint inflammation with swelling, pain & tenderness along with limited range of motion can also accompany dactylitis. In some cases, dactylitis not only affects hands or feet, but also an elbow or a knee. Inflammation, resulting from arthritis & dactylitis can most often be controlled with anti-inflammation medications like aspirin & ibuprofen.
• Bacterial Infection
Pneumonia, which is a lung infection is most common among children with sickle cell disease & is also a major reason for their hospitalization. However, pneumonia can be quite slow to respond to antibiotics. Type of bacteria which frequently causes pneumonia is known as pneumococcus. Pneumonia in part is caused due to increased susceptibility to this type of bacteria, especially when spleen is functioning poorly. In such cases vaccination against pneumococcal infection is commonly recommended. Children with sickle cell disease are also at risk of infection of brain & meningitis (spinal fluid). Bacteria are the frequent cause of this infection including Haemophilus & Pneumococcus bacteria. Moreover, children with sickle cell disease are at risk of an unusual type of bone infection known as osteomyelitis. Typically, this infection is from a bacteria known as Salmonella. Bacterial infections at times can be serious & overwhelming for patients with sickle cell disease. Early detection along with antibiotic treatment is the key to minimizing complications. Children with sickle cell disease must therefore be evaluated by doctors whenever they develop fever or any other signs of infection like unexplained cough or pain when they appear. However, over time the spleen of sickle cell anemia patient can become damaged & stop working & which as a result increases risk of developing many other severe infections.
• Liver Congestion & Splenic Sequestration
It has been clearly demonstrated that liver, especially the spleen, is a very active organ which is involved in removing sickle red blood cells from blood circulation of people with sickle cell disease. Moreover, this process is also found to accelerate suddenly & this sudden pooling of blood within spleen is referred to as splenic sequestration. Splenic sequestration is found to cause severe anemia in patients & which can even prove to be fatal. Spleen therefore is commonly enlarged & which is known as splenomegaly in younger children affected by sickle cell disease. When spleen is repeatedly injured from damage due to impaired blood supply, it gradually starts to shrink along with scarring. Impairment of normal functioning of spleen generally increases tendency to get affected with bacteria. This can result in extremely severe anemia & even death in some cases. Such affected patients can develop shocks & even lose consciousness at times. Blood transfusion along with fluids can be critical when this occurs. Hepatomegaly or liver enlargement generally occurs when it gets congested with red blood cells. Most often, the liver which is form can eventually turn to become tender. Impaired function of the liver can result in jaundice whose prominent symptom is yellowing of the eyes. Gallbladder, which usually drains bile from liver, can get filled with gallstones at this point of time. Inflammation of gallbladder which is known as cholecystitis, can result in causing vomiting & nausea & can cause vomiting & nausea & which calls for surgical removal.
• Injury to Heart & Lungs
Apart from pneumonia, lungs of sickle cell disease can also be injured due to inadequate circulation of blood which can cause areas of tissue death. This type of lung damage can be very difficult to distinguish from pneumonia & is medically termed as acute chest syndrome. Such localized areas of lung tissue damage are usually referred to as pulmonary infarcts. Pulmonary infarcts most often require to undergo special x-ray tests using injection of dye into affected areas known as angiograms, in order to be diagnosed. Moreover, repeated pulmonary infarcts can lead to scarring of lungs in children with sickle cell disease by the time they turn into adolescents. Heart of children with sickle cell disease is frequently enlarged due to anemia. Murmurs & rapid heart rates are quite common. Heart muscle is also found to be injured by iron depositing & infarcts in muscles from leaks due to ruptured red blood cells. Heart muscle weakens over time & pumping of blood from the heart eventually gets poorer by the day. Injuries to heart & lungs are treated according to specific type of damage& degree of impairment of functioning of organs. There may also be requirement of supplementary oxygen. Blood transfusions can also at times help prevent further damage to heart & lung tissue. Heart failure may need medications to assist heart in effectively pumping blood to the body.
• Ulcers in Legs
Legs of patients with sickle cell disease are susceptible to ulceration & skin breakdown. This is largely as a result of stagnant flow of blood caused by sickled red blood cells. Injury to ankles or skin of legs can also promote ulceration & skin damage. However, most commonly leg ulcers occur in adult patients & these usually form over ankles & sides of lower legs. These ulcers can often become severe & even encircle the leg & are prone to infection as well. Ulcers in leg can become chronic & resistant to a variety of treatments. Topical creams & oral antibiotics are often used for treatment. Careful dressing changes, elevation of leg & many other topical therapies can prove helpful. When some ulcers are resistant, skin grafting is normally recommended, but this may in cases be compromised by impaired healing.
• Bone Infarcts & Aseptic Necrosis
Inadequate circulation of blood is characteristic to sickle cell disease. It also causes areas of death of bone tissue known as bone infarction. Localized bone death or aseptic necrosis results of inadequate supply of oxygen to bone. This is commonly referred to as osteonecrosis. Virtually any bone can be affected, but the most common bones include the arms, thighs & legs. This can also permanently damage the knees, hips or shoulders as well. Tenderness, disability & pain are frequent signs of aseptic necrosis. Bone infarcts which are painful can however be relieved by rest & pain medications. However, aseptic necrosis can permanently damage large joints like shoulders or hips. Nevertheless, local pain can be effectively relieved & worsening of the condition be prevented by avoiding bearing of weight. Moreover, total joint replacement can restore the required function in cases of more severe damage.
• Damage to Eyes
Critical area of the eye which normally senses light is known as the retina. Retina is located at the back of the eye & is nourished by several tiny blood vessels. Impairment of blood circulation due to sickling of red blood cells eventually results in damage to retina & which is known as retinopathy. This mayeventually result in partial or total blindness. Known as retinal hemorrhage, bleeding can also occur in the eye & subsequently result in detachment of the retina. Retinal detachment may then lead to complete blindness. Once blindness has occurred, it usually leads to permanent vision loss. Preventive measures like laser treatments can prove to be useful in case bleeding inside eye & retinal detachment are detected early.
• Other Features
Additional features of sickle cell disease include weakening of bones due to osteoporosis, damage & infection to kidneys & damage to the nervous system. Moreover, osteoporosis can also lead to severe pain in back & deformity from collapse of vertebrae. Damage to kidney can often lead to poor kidney function along with an imbalance of acidity & blood sodium as well as bleeding in urine. Poor kidney function can also cause pelvic pain which may even require hospitalization along with antibiotic treatment. Injury to nervous system may result from sickle cell disease or meningitis. Poor blood circulation within brain can cause convulsions, stroke & coma as well. Damage to brain from stroke is likely to cause permanent loss of function to areas of body. Intravenous fluids & transfusion of blood in such situations is critical. Medications which reduce chance of seizures are also added at times. These strokes often are found to result in long-term impairment of function & physical therapy, occupational therapy & speech therapy can be very helpful. Priapism is an abnormally persistent type of erection of penis in the absence of sexual desire & which can occur in people with sickle cell disease. However, priapism can lead to damage of affected tissue & impotence.
Prognosis for Sickle Cell Disease Patients
Life expectancy of people with sickle cell disease is reduced. However, some patients can remain for years without symptoms, while others fail to survive infancy or even early childhood. Nevertheless, sickle cell disease patients with optimal management can now effectively survive beyond the fourth decade. But then, most sickle cell disease patients suffer intermittent pain crises including fatigue & bacterial infections which eventually lead to progressive tissue & organ damage. Impaired growth & development as such is the end result of physical & emotional trauma which is endured by children suffering from sickle cell disease. Most common causes of death among sickle cell disease patients include stroke, bacterial infection, bleeding inside heart, kidney, brain or liver failure. Risk of bacterial infections however diminishes after 3 years of age, in spite of the fact that it is the most common cause of death among sickle cell anemia patients at any age. This is why any sign of infection in sickle cell anemia patient must essentially be reviewed with doctors so as to prevent damage & save lives as well. Interestingly, it is found that sickle cell gene protects against malaria infection & which makes these patients partly protected against malaria infection. Geographic distribution of sickle cell gene is quite similar to malaria infection. This is a lethal condition which threatens life but there are selective advantages to carrying a sickle cell trait if the person is residing in regions of the world where malaria is common. This very advantage of people with sickle cell trait over the non-carrier of gene can possibly explain as to why sickle cell disease did not disappear from world even though it is lethal. However, sickle cell gene is not a ‘black gene’ as it is commonly perceived. It is only found to disproportionately occur in black population. Whenever a black person carrying sickle cell gene has children with non-black individual, their children may inherit sickle cell gene regardless of race. Moreover, there are people of many other races who are found to carry sickle cell gene. Research nowadays is examining ways to promote development of fetal hemoglobin which delays development of sickle cells in the newborn. Bone marrow implant is one such way which is used for sickle cell disease patients having a sibling donor. Future treatment options may also involve genetic engineering through which a cure can be achieved. Genetic counseling may eventually be helpful for parents & families to prevent sickle cell disease from occurring as sickle cell disease is an inherited disease where both parents must be carriers of sickle cell gene for the child to be affected by sickle cell disease. Whenever both parents are carriers there is a 50 percent chance of the child also being a carrier & 25 percent chance of inheriting both genes from parents in order to be affected by sickle cell disease.
Demographic Which is Most Affected by Sickle Cell Disease
Approximately, over 70,000 to 100,000 Americans are found to be having sickle cell disease. This is the most common form of inherited blood disorder which causes production of abnormal hemoglobin. Healthy red blood cells are flexible & can therefore move through the tiniest blood vessels. Sickle cells can however get stuck & stop blood flow to specific organs & cause conditions for stroke, acute chest syndrome, organ damage & other disabilities including premature death in some cases. Moreover, there are variations of sickle cell disease which is called Sickle Thalassemia or Sickle C & which is also a serious condition but less severe. People having sickle cell disease will eventually pass one sickle cell gene to their children as well.
• Sickle Cell Trait
This is an inherited blood disorder which affects almost 8 percent of African-Americans. Unlike sickle cell disease in which two genes are found to cause production of abnormal hemoglobin, people with sickle cell trait carry only one defective gene. Typically, these people live normal lives without any health problems relating to sickle cells. It is quite rare that extreme conditions like high intensity physical activity & severe dehydration will lead to serious health problems including sudden death among people with sickle cell trait.
• Risk Factors Associated with Sickle Cell Disease
Since sickle cell disease symptoms begin to appear by four months of age, early diagnosis is quite critical to treatment. Therefore, all newborns in United States are now tested for sickle cell disease. Sickle cell disease can also be identified prior to birth by testing amniotic tissue or fluid from placenta. People carrying sickle cell gene must seek genetic counseling prior to pregnancy so as to discuss options that are available.
Bone Marrow Transplant (BMT) for Treating Sickle Cell Disease
Bone marrow or stem cell transplants have been in used as treatment & cure for a variety of cancers, blood & immune system diseases for several years. Doctors have developed studies to treat children having severe sickle cell anemia with bone marrow transplants.
• How do Bone Marrow Transplants Work?
Bone marrow produces red blood cells containing hemoglobin S in people suffering from sickle cell disease. This eventually leads to complications of sickle cell anemia.
• In preparation for bone marrow transplant, strong medicines known as chemotherapy are used in order to weaken or destroy patient’s own stem cells, bone marrow & the immune system. This is usually done so that the patient does not reject new blood cells which are coming from the donor.
• Patient’s bone marrow is subsequently replaced with new blood-forming stem cells from donors who are not having sickle cell anemia. The donor can be with normal hemoglobin or with sickle cell trait. The actual bone marrow transplant is administered like blood transfusion through an IV line.
• New bone marrow will now produce red blood cells which are healthy as they do not contain lot of hemoglobin S.
• Who Can Donate Stem Cells for Bone Marrow Transplants?
There are 3 main types of stem cell donors for bone marrow transplant.
• Matched Related – This can be a brother or sister who is having the similar bone marrow type & the same as father & mother. Brothers & sisters are normally matched through special blood tests known as HLA typing.
• Matched Unrelated – This includes volunteers who are having the same type of bone marrow as the patient. These types of donations are usually matched through national organizations which match patients & donors having the same type of bone marrow.
• Haploidentical – These include half matched family members like the mother or father. This donation type is still under experimental stages & is performed mostly as a part of research studies.
Stem cells nowadays can also be obtained from donor’s peripheral blood (blood in veins) or bone marrow. Moreover, in some cases stem cells are also collected from the umbilical cord of the patient at the time of birth.
Benefits of Bone Marrow Transplant
Bone marrow or stem cell transplant presently is the only treatment which is available which can cure sickle cell anemia. When bone marrow transplant is successful it can effectively cure sickle cell disease.
Potential Risks of Bone Marrow Transplant
Potential risks associated with bone marrow transplant include the following.
• Infections
Chemotherapy, which is part of the treatment, lowers white blood cells in the body which normally fight & protect the body from infections. Eventually, this puts the sickle cell disease patient at high risk of infections & which can be caused by viruses, fungi or bacteria. Medications are given to fight & prevent germs causing infections in this situation. However, infections usually do not do not respond well to drug treatment at this point of time & can lead to 5 – 10 of deaths among sickle cell disease patients.
• GVHD or Graft-Versus Host Disease
This is a reaction of the body which occurs when immune cells of donor graft cells sense that cells of sickle cell disease patient host cells are foreign & therefore attack them. This can potentially be a serious side effect of bone marrow transplant. GVHD is found to occur in up to 0 percent of the sickle cell anemia cases among patients who undergo matched related type of bone marrow transplants. This percentage can also be higher among bone marrow transplants using other types of donors. Moreover, this condition can be acute if it is occurring less than 100 days following bone marrow transplant or chronic if it is occurring more than 100 days following bone marrow transplant. Nevertheless, it may cause damage to liver, intestinal tract & skin of the patient undergoing treatment. Drugs are normally given to patients in order to limit or prevent GVHD. These drugs generally increase the risk of infection & when GVHD does not respond to treatment, it may lead to organ damage or even death in a percentage of sickle cell disease cases.
• Graft Failure
Generally, there is a 10 percent risk that the newer bone marrow transplant from a matched family donor will fail. However, chances of graft failure are higher with involvement of other types of donors. This in fact means that the sickle cell disease patient will not be able to produce platelets, red blood cells or white blood cells. Typically, the bone marrow transplant in such conditions will be required to be repeated. Stem cells which were collected from the sickle cell anemia patient prior to bone marrow transplant can be given back to the sickle cell disease patient. This will be able to restore the original bone marrow of the patient & which will mean that the sickle cell disease has come back.
• Veno-Occlusive Disease or VOD
Blood vessels which lead into & pass through liver might suffer damage following bone marrow transplant. This is usually caused by chemotherapy & may eventually lead to swelling & causing severe damage to the liver. Chances of severe VOD are about 5 percent, which means that VOD may occur in about every 1 out of 20 sickle cell anemia cases.
• Problems with Nutrition
Since stomach & intestines are very sensitive following chemotherapy, it may cause mouth sores, vomiting, nausea, diarrhea & loss of appetite to occur in sickle cell disease patients treated with these chemotherapy drugs. Nutrition therefore must be typically given through veins until the patient is able to normally eat & digest.
• Lower Blood Count
Sickle cell anemia patients usually require transfusions of red blood cells & platelets while they are waiting for the newer stem cells to start producing normal red blood & other types of cells.
• Social & Emotional Concerns
Bone marrow transplant is a challenging procedure, both for the patient & family members. Routine of patients may change for some time as they will be away from home & isolated from friends, relatives & school. However, family holds the key to supporting the sickle cell anemia patient through the bone marrow transplant procedure. Average time spent by patients in hospital is between 4 – 6 weeks.
• Infertility
Most patients receiving bone marrow transplant will typically not be able to have children of their own in future. This is normally a side effect of drugs which are used during preparation for the bone marrow transplant. However, there have been some cases of sickle cell anemia patients who were still able to conceive children even after undergoing bone marrow transplant.
Requirements for Bone Marrow Transplant
There are two major requirements which must be met for a sickle cell anemia patient to undergo bone marrow transplant.
• Firstly, a person must be identified as the best & most suitable donor. Blood test will be able to determine as to which is the best match.
• Secondly, following identification of the most suitable donor, both the sickle cell anemia patient & the donor will have to undergo pre-transplant evaluations of kidneys, lungs, heart & other organs. This will be followed by interviews with psychologists & social workers who are an important part of the bone marrow transplant procedure
Is Bone Marrow or Stem Cell Transplant the Only Treatment for Sickle Cell Anemia?
Yes, as of now bone marrow transplant is the only cure for sickle cell anemia. Results of several studies reveal that bone marrow transplants from matched related donors offer about 80 percent chance of cure from sickle cell disease. Other treatment choices available for sickle cell anemia patients include chronic red blood cell transfusions & hydroxyurea drug. However, these treatment options can lessen complications associated with sickle cell anemia, but they are not able to cure the disease itself.
Types of Bone Marrow Transplants
Types of bone marrow transplants include the following.
• Syngeneic
This is when the donor is an identical twin of the sickle cell anemia patient. This is one of the simplest sources of obtaining stem cells for bone marrow transplant. Syngeneic transplants are the best & least complicated bone marrow transplants because there is no risk of rejection, tumor in marrow or GVHD – graft-versus-host disease. Return of immune system & blood cell recovery is also prompt. However, the only disadvantage of syngeneic transplant is lack of graft versus leukemia (GVL) effect relating to allogeneic transplants which in fact help reduce tumor relapse.
• Allogeneic
Allogeneic donor is the one other than the sickle cell disease patient. Allogeneic bone marrow transplants have lower risk of tumor relapse due to the GVL effect. However, when the new transplanted immune system recognizes the patient as foreign (GVHD), immune deficiency & graft failure, are potential problems associated with this type of bone marrow transplant. Allogeneic donors are usually chosen based upon a blood test which is conducted for human leukocyte antigens or HLA in short. HLA antigens are part of the biological process which allows immune cells of patients to differentiate between self & cells from other people or foreign organisms. Matched donor can either be a relative, which is usually a brother or sister, or unrelated individuals sharing all 1 HLA antigens with sickle cell anemia patients. All allogeneic bone marrow transplants have historically utilized matched donors because mismatched HLA were generally associated with high risk of GVHD.
• Autologous
The patient’s own peripheral blood or bone marrow is used in this type of bone marrow transplant procedure. Like syngeneic bone marrow transplant, there is no risk of rejection (GVHD) & GVL effect is also absent in autologous bone marrow transplants. Additional concern of tumor contamination of transplant is however present, although this is a relatively minor concern for certain solid tumors but proves to be a major problem for all types of blood cancers including some solid tumors. Doctors have however pioneered methods to remove or ‘purge’ tumor cells from autologous bone marrow transplants including methods meant to reduce relapse which is similar to allogeneic GVL effect
.
• Haploidentical
Several sickle cell anemia patients in need of bone marrow transplant may not have a unrelated donor matched family member. In such cases a half-identical or haploidentical related donors can provide similar outcomes which are seen with matched bone marrow transplants. Children & parents & about half siblings are found to be half-matches. Ability to perform haploidentical bone marrow transplants has in fact revolutionized bone marrow transplantation techniques so that almost everyone now requiring a stem cell transplant can get one.
• Umbilical Cord Blood
Partially-matched cord blood is another source of stem cells required for bone marrow transplantation. Umbilical cord blood is a type of bone marrow transplant which has essentially become standard-of-care especially for children needing stem cell transplantation. However, due to small size of umbilical cord blood transplants, this procedure is still under research for adults.
Recovery & Precautions Following Bone Marrow Transplants
After newer cells engraft & begin to create & grow new blood cells for the body, blood cell counts of the sickle cell anemia patient will begin to improve alongside the immune system becoming stronger. This is usually the time of transition in the patient’s recovery. Bone marrow transplant patients at this point of time would probably leaving the hospital, although they would still be paying frequent outpatient care visits at the transplant center. Nevertheless, bone marrow transplant patients will still be weaker than normal for many more months to come. Risk of complications from stem cell transplant is the highest during the first 100 days after the procedure. The transplantation team will continue caring for the patient & closely watch them for any signs of infection & other problems. They will also provide guidelines for patients to follow in order to help prevent occurrence of infections. However, if sickle cell disease patients have any symptoms, they should immediately contact the doctor.
• After Discharge from Hospital
At times during the first 100 days following bone marrow transplant when the sickle cell anemia patient has engrafted, they are able to take oral medications & will probably allowed discharge from the hospital. Subsequently they will be received as outpatients in days to come. Henceforth, the patient will play an important role in their own healthcare. However, bone marrow transplant patients will need to pay attention towards the following when they leave the hospital.
• BMT patients must effectively follow guidelines given to them regarding reducing risk of life-threatening infections & associated complications.
• Take all medications exactly as prescribed by doctors.
• Eat healthy. Follow instructions given by the healthcare team regarding food handling & safe eating. This will help BMT patients to reduce risk of infection & regain strength at the same time.
• Immediately call on the doctor when BMT patient is experiencing symptoms or signs of infection.
Each patient will however have a different experience while transitioning to outpatient care. For some BMT patients this transition will be smooth, while several others may experience side effects, symptoms or complications which require re-admitting in the hospital. However, it is common for bone marrow transplant patients to re-enter the hospital so as to be treated for side effects & symptoms following bone marrow transplant. Of course, not all BMT patients are required to reenter the hospital. Bone marrow transplant patients will often visit the outpatient clinic, perhaps daily, in the first few weeks or months after discharge from hospital. They should therefore expect to stay near the transplant center for treatment for at least 100 days following discharge & until all complications are resolved. Since the sickle cell disease patient will be tired after bone marrow transplant & the caregiver would be looking after their daily requirements, here are some suggestions which can be taken up & which can be taken up so as to rebuild the strength & health of the SCD patient.
• The SCD patient must get enough rest. They would normally be tired as the body would be working hard so as to recover from intense treatment which they had received during the bone marrow transplant.
• Sickle cell disease patient must get some exercise everyday as per their ability to do so. Several people who have undergone bone marrow transplant say that it helped them get up & walk every day, even when they were able to only walk a short distance. However, over a period of time the patient’s strength would grow & they will be able to do much more.
• It would be wiser to be patient over time & allow the body to heal.
• When bone marrow transplant patients finally leave the hospital, they & the family members would now rely on plans for caring & housing they had made before undergoing the BMT procedure.
• Infections & Bone Marrow Transplant
The immune system would be very weak following bone marrow transplant. This is caused by both, preparative regimen which the patient receives prior to bone marrow transplant & drugs which were prescribed following bone marrow transplant, like those meant to prevent complications like graft-versus-host disease. Graft-versus-host disease (GVHD) is a common complication of bone marrow transplant patient receiving stem cells from an unrelated donor. Factors, which a bone marrow transplant patient must bear in mind about infections, are listed below.
• Most infections are found to happen within the first 100 days after bone marrow transplant. However, these remain a risk until the patient’s immune system is weak.
• These infections can be very serious & life-threatening is quite a few cases. Nevertheless, the transplant healthcare team will keep a close watch & look out for signs of infections.
• The BMT patient is most likely to receive further medications in order to reduce risk of infections.
The BMT patient & the caregiver’s awareness of signs & symptoms of infection is the first line of defense & the most important against serious & life-threatening infections after they are discharged the hospital. BMT patients having any sign of infection post discharge, like for example fever, must let the transplant healthcare team know right away since it is very important to quickly treat these infections. The immune system of the patient will not be in full strength following bone marrow transplant for as long as a year or two. They will still need to take anti-infection drugs up till then. GVHD patients may have weak immune systems for even a longer period of time due to the medicines used for treating them.
• Acute Graft-Versus-Host Disease
Graft-versus-host disease or GVHD is a common complication following allogeneic bone marrow transplant. This is a type of bone marrow transplant which involves cells from a family member, cord blood or an unrelated donor. Immune cells from cord blood or donated marrow in GVHD attack the body of the BMT patient in this case. GVHD which appears within the first 100 days following bone marrow transplant is known as acute GVHD. GVHD which occurs later than this time frame is known as chronic GVHD.
India is a Hub for Affordable Bone Marrow Transplant
Bone marrow transplant in India in fact costs just a fraction of what it takes in other countries. Moreover, there are very few centers across the world where this procedure can be performed are not enough dedicated professional medical staff are available. Another aspect of bone marrow transplant is a procedure where newer cells are introduced into damaged tissue so as to treat injury or disease, has shown considerable promise in treatment of various types of diseases, including certain types of cancers. Nevertheless, there are about 10 to 11 centers in India where bone marrow transplant procedures are performed.
• Cost of Bone Marrow Transplant in IndiaWhile bone marrow transplant can cost a whopping $223,000 in other countries depending upon the type of procedure, in comparison in India it costs almost 80 percent less & is much cheaper depending upon the type of procedure. Bone marrow transplant has shown 50 percent success in treatment of certain types of cancers including other major conditions like aplastic anemia condition where bone marrow cells do not produce sufficient newer cells to replenish older blood cells & beta thalassemia which is a genetic disorder of the blood. Bone marrow transplant has also shown 70 to 80 percent success rates in treatment of non-malignant diseases like aplastic anemia. In a few cases of bone marrow transplant, despite matching with donors, the patientansplants whiloe is found to reject the graft. These cases then involve a lengthy process of giving immunosuppressants or medications which help prevent organ rejection in case of transplants while reducing inflammation as well. Moreover, in some cases steroids are also given to BMT patients to help in accepting the transplant.
Indian Hospitals at the Forefront of Bone Marrow Transplant
• Medanta – The Medcity at Gurgaon
Medcity is perhaps one of the largest multi-super specialty hospital facility located in Gurgaon near Delhi. This is in fact a bustling town in the NCR which was founded by the eminent cardiac surgeon Dr. Naresh Trehan. Spread across 43 acres of land, Medcity includes a research center, medical & nursing schools & has over 250 beds including 350 critical care beds & 37 operating theatres catering to 20 specialties. One of its kind facility across the world, Medcity provides access to affordable healthcare.
• Manipal Hospitals at Bengaluru
Most adults identified with type of bone cancer are eligible for bone marrow transplant. However, their cardiac rejection rate should either be less or equal to 45 percent. Other criteria which determine eligibility for bone marrow transplant for patients include the LFTs & HLA matching. Moreover, a series of tests are also conducted on patients in order to determine that they in fact require bone marrow transplant. It is an accepted fact that patients with bone cancer usually do well following bone marrow transplantation. Apart from bringing the patient’s physical activities to normal, BMT is also considered as a permanent solution to problems and/or complications in the stem cells of patients like in case of sickle cell disease. At Manipal Hospitals in Bengaluru, bone marrow transplantation is used to treat the following types of diseases.
• Malignant Diseases – These include Leukemia (Acute Myeloid & Acute Lymphoblastic leukemias).
• Benign Diseases – Like Thalassemia Major, Severe Aplastic Anemia & Immune Deficiency Disorders.
• Relapsed Non Hodgkin’s & Hodgkin’s Lymphoma
• Kokilaben Dhirubhai Ambani Hospital at Mumbai
Bone marrow transplant unit at Kokilaben Dhirubhai Ambani unit at Mumbai is dedicated to provide outstanding care & support, especially to pediatric patients who can benefit by BMT therapy. This program is meant to providing bone marrow transplant as a treat option for a wide spectrum of congenital disorders of infants & young adults including acute & chronic blood conditions. Expert team of professionals at Kokilaben Dhirubhai Ambani Hospital specializes in performing autologous & allogeneic bone marrow transplants including umbilical cord blood transplants, peripheral stem cell transplants while providing the best possible care to international patients. HEPA filters at the Kokilaben Dhirubhai Ambani Hospital’s bone marrow transplant unit provide air which is free of microorganisms within the premises. Bone marrow transplantation which is also known as hematopoietic stem cell transplant is useful in increasing remission or chances of cure in some benign blood disorders & blood cancers as well. BMT treatments at Kokilaben Dhirubhai Ambani Hospital usually involve intense chemotherapy which is followed by infusion of stem cells. However, most bone marrow transplant treatments require close nursing & exceptional medical care lasting for a number of weeks during recovery.
• Kidwai Memorial Hospital at Bengaluru
Named after Mr. Rafi Ahmed Kidwai, Kidwai Memorial Institute of Oncology is sprawled over 20 acres of land at Dr. M. H. Marigowda Road in Bengaluru. Established on 26th June, 1973, this institution became autonomous on 8th January, 1980. Government of India has accorded status of Regional Cancer Center to Kidwai Memorial Hospital on 1st November, 1980 when it became the 11th in line, Regional Cancer Center in the country. Indian Council of Medical Research has recognized Kidwai Memorial Hospital as a referral research institution. From 1980 to 2001, the face of non-descript Kidwai Memorial Cancer Hospital has changed into a well known major & model comprehensive regional cancer research center offering cancer treatments including bone marrow transplant for sickle cell disease alongside sophisticated diagnostic & treatment services to an ever increasing number of cancer patients from the entire country & abroad. Kidwai Memorial Cancer Hospital in Bengaluru is only next Tata Memorial Hospital in Mumbai in terms of staff, equipment, accommodation, organization & patient turnover.
• Fortis Memorial Research Institute at Gurgaon
The hematology department at Fortis Memorial Research Institute at Gurgaon has an expert team involved in diagnosis & treatment of blood diseases. These hematologists evaluate & treat patients suffering from various conditions including sickle cell anemia, reduced or increased white blood cells, decreased or increased platelets, enlarged spleen or lymph nodes & clotting & bleeding disorders of the blood. This department of hematology ar Fortis also has experts who treat blood cancer conditions like multiple myeloma, lymphoma, leukemia & other disorders of the blood.
• Christian Medical College at Vellore
Hematology department at Christian Medical College Hospital at Vellore looks after patients with problems in the blood. This generally includes leukemia, sickle cell disease & congenital diseases like hemophilia & thalassaemia. Common blood related problems which are treated at this hospital include the following.
• Platelet related & bleeding disorders like hemophilia
• Blood cancers affecting lymph nodes like lymphomas, leukemia & multiple myeloma
• Bone marrow failure syndromes like sickle cell disease & aplastic anemia
• Genetic problem of the blood like Thalassaemia
Bone marrow transplant takes cells from inside bones of a healthy individual & transfers them to the patient who is sick. Bone marrow is where the platelets, red blood corpuscles & white blood cells are produced. Bone marrow transplantation at Christian Medical College Hospital at Vellore are performed for people with sickle cell disease, aplastic anemia, myeloma, thalassaemia & leukemia.
• BLK Centre at New Delhi
BLK Centre for Bone Marrow Transplant or BLKBMT in short, is the largest facility in India & among one of the biggest in entire Asia. This is a standalone dedicated facility which is equipped with an ultra-modern infrastructure & internationally trained professional staff alongside widely experienced faculty. BLKBMT is supported by state-of-the-art transfusion & laboratory services along with fully equipped radiation oncology unit which is having facilities for total body irradiation. This center offers both autologous & allogeneic transplants using cord blood stem cells, peripheral blood stem cells & bone marrow for various malignant & benign blood disorders for advanced pediatric solid tumors, multiple myelomas, lymphomas, leukemia, aplastic anemia, thalassaemia & sickle cell disease. BLKBMT by now has performed over 500 bone marrow transplants within a short period of time.
Departmental Highlights at BLKBMT
• BLKBMT is one of the largest centers of its kind across Asia
• BLK Centre has performed maximum number of transplants in North India
• Each & every room at BLK Centre is supported by HEPA filter with triple level air filtration
• Bone marrow transplants are routinely performed here for children & adults as well
• BLKBMT is credited with Delhi’s first Match Unrelated Donor (MUD) Transplant
Bone marrow transplantation at BLKBMT is a procedure wherein stem cells from bone marrow produce various types of blood cells like platelets, white blood cells & red blood corpuscles are injected into a recipient. These stem cells are often referred to as hematopoietic stem cells. Hematopoietic stem cells nowadays are also obtained from umbilical cord or peripheral blood after it has been treated with certain growth factors. The term Hematopoietic Stem Cell Transplantation is now much preferred to Bone Marrow Transplantation since it includes other sources of hematopoietic stem cells as well.
• Apollo Hospitals
Blood & bone marrow transplant center at Apollo Hospitals in India have performed more than 700 bone marrow transplants with excellent success rates. Apollo Hospitals is a trusted name in India & is an excellent place for international patients to undergo bone marrow transplantation. Apollo Hospitals maintains a highly qualified BMT team alongside a very stringent infection control system which is highly critical for BMT patients. BMT treatments are available for patients at Apollo Hospitals in Chennai, Kolkata, Ahmadabad, Hyderabad, & New Delhi.
Why Choose AVAN MediTour to Undergo Bone Marrow Transplantation?
AVAN MediTour provides outstanding opportunities for bone marrow transplants in the best hospitals for BMT in India. Alongside 24/& assistance & call & electronic mail services which patients can rely upon, AVAN MediTour is associated with the best bone marrow transplant doctors who are some of the best experts available in India. Patients associated with AVAN MediTour are assured of receiving affordable, seamless, high quality, transparent & hassle-free extensive range of bone marrow transplant treatments to overcome medical problems like multiple myelomas, neuroblastoma, sickle cell disease, leukemia & other associated genetic disorders.
Sickle Cell Disease across the World
Sickle cell anemia is most common among Africans & African-Americans. This is an inherited blood disorder which is also found in other ethnic & racial groups among people from South & Central America, Caribbean, India & several other Mediterranean countries. Sickle cell anemia typically causes the normal round & flexible red blood cells in body to abnormally shape like crescent moon or sickle shaped. These damaged structures disable smooth travel of red blood cells within the smaller blood vessels & thereby quite often block normal blood flow while triggering loss of essential oxygen supply to affected tissues. Furthermore, sickled red blood cells only live for about 10 to 20 days against the normal 120 days lifespan enjoyed by regular red blood cells. Alongside anemia, sickle cell disease causes severe pain. SCD can also cause permanent damage to kidneys, liver, spleen, lungs, brain & heart as well. However, sickle cell anemia is not a contagious disease, but there are children who are born with this medical condition. Sickle cell disease is typically found to happen a child inherits two sickle hemoglobin S genes, one each from the father & mother.
Affordable Cost of Bone Marrow Transplant in India
India has emerged as a globally specialist destination for bone marrow transplant procedures. Moreover, cost of bone marrow transplantation in India is affordable & just a fraction of what a sickle cell disease patient would normally have to pay in western developed countries like Germany, UK, Canada & the United States. Offering high technology medical solutions to international patients with healthcare problems, India today is one of the most favored global healthcare destinations. Another plus for the Indian medical tourism success story is that, apart from affordability & world class facilities, success rates for most medical procedures in India are at par with the best in the world. Moreover, it is not just the doctors who are able to communicate in English, nurses & the other professional staff manning hospital facilities in India, also speak the language so as to provide a cozy & familiar environment for an international patient during recovery following surgical procedures.
Inclusions and Exclusions
INCLUSIONS
1. Airport Pick-up on Arrival in India2. Airport Drop on Departure from India
3. Cost of initial Evaluation and Diagnosis
4. Cost of the Surgery or Treatment
5. Cost of applicable one implant/prosthesis
6. OT Charges and Surgeon’s Fees
7. Consultation Fees of the Doctor for the concerned specialty
8. Nursing and Dietician’s Charges
9. Hospital Stay for the specified number of days in the respective room category as mentioned against the package
10. Hospital stay includes stay of the patient and one attendant for the duration of stay mentioned against the package
11. Routine investigations and medicines related to the surgery or treatment.
12. Food for the patient and the attendant for the specified number of days as mentioned against the package
13. Travel Assistance/Medical Visa Invite/FRRO/ Visa Extensions
14. Assistance in finding right budget hotel or guest house accommodation.
15. Issuing Invitation Letter for Medical Visa.
EXCLUSIONS
1. All expenses for stay beyond the specified number of days2. Cross Consultations other than the specified specialty
3. Use of special drugs and consumables
4. Blood products
5. Any other additional procedure
6. Post discharge consultations, medicines, procedures and follow-ups
7. Treatment of any unrelated illness or procedures other than the one for which this estimate has been prepared
8. Travel Expenses and Hotel Stay
DISCLAIMER:
* Quote given is ONLY for the treatment in the hospital and DOES NOT include food as well as the accommodation cost outside the hospital.
* The quote may vary in case of co-morbidities, which are associated medical conditions and an extended stay.
* The treatment suggested is as per the information and reports provided to us. The line of treatment may differ according to the additional and comprehensive details asked by our consultants.
* The prices quoted are only indicative and may differ. They can be confirmed only after the patient is assessed by a doctor.
* The complete treatment cost has to be deposited in advance after the finance counseling for the patient is done at the hospital